If you happen to click here and listen to B. B. King sing “The Thrill is Gone,” you might notice that he does not look happy. Nor does he sound happy. And he’s sweating. A lot! He says he’s free, but I somehow doubt it.
What happens when the thrill is gone? That’s a central question for addiction, as most of us know first-hand. In fact, what if the thrill was never there to begin with…?
I said I’d report to you on everything I learned at the conference on behavioral addictions in Budapest last month. First I reported on the common denominator, OCD-type states in brain and behaviour, then I tried to specify the key difference between substance and behavioral addictions, then came Elizabeth’s guest post comparing food and drug addiction, and now here’s Part 4: the genetics of thrill-seeking.
On day 2 of the conference, once my brain was seriously sweating, I met the guy who coined the term Reward Deficiency Syndrome (RDS). His name is Kenneth Blum, and he’s a smallish wiry guy, very intense, seemingly dour, but flashing the occasional dry smile. Here’s his hypothesis:
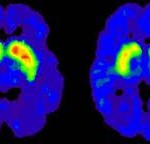
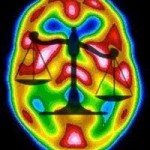
When we take drugs, or do whatever it is we’re addicted to, the brain systems that “light up” include dopamine circuits in the striatum and its neighbours. No surprise there. Blum lists half a dozen dopamine receptors that get in on the act. But the lead role goes to the D2 receptor — which controls the amount of dopamine available to synapses all over the frontal cortex and striatum. The D2 receptor is involved in attention, motor control, motivation….lots of pretty important stuff. Here’s a detailed description. So what happens when the D2 receptor population isn’t quite normal (e.g., too many or too few)? What happens is that you are more likely to suffer from a whole host of things, including OCD, ADHD, schizophrenia, and — you guessed it: addiction. Addiction to drugs, booze, gambling — that receptor has a lot of connections with the underworld of our psyches.
The problem is that the gene that’s responsible for growing D2 receptors, while we’re in the womb, has got different variants (like many genes), and one of those variants (allele A1) causes an overall reduction in the number of D2 receptors. There’s lots of evidence that addiction runs in  families, and I’ve usually been reluctant to pin it all on genetics. Why? Because most scientists agree that there’s no single gene or cluster of genes that causes addiction; genetic predictors of addiction usually depend on personality factors, like impulsivity; and there is so much in behaviour and experience that can bridge generations — for example, you hardly need a genetic boost if your dad is an angry drunk and your mom is seriously depressed. But Blum cites some pretty convincing research showing that addictions shared across generations (like father, like son) correspond with this nasty dopamine allele. It shows up in more than one generation! That is to say the allele gets passed down, along with the silverware and the porcelain figures nobody wants.
families, and I’ve usually been reluctant to pin it all on genetics. Why? Because most scientists agree that there’s no single gene or cluster of genes that causes addiction; genetic predictors of addiction usually depend on personality factors, like impulsivity; and there is so much in behaviour and experience that can bridge generations — for example, you hardly need a genetic boost if your dad is an angry drunk and your mom is seriously depressed. But Blum cites some pretty convincing research showing that addictions shared across generations (like father, like son) correspond with this nasty dopamine allele. It shows up in more than one generation! That is to say the allele gets passed down, along with the silverware and the porcelain figures nobody wants.
In a nutshell, some people have fewer D2 receptors, like maybe 40% fewer in some brain areas like the nucleus accumbens. So these people are not as excited about reaching their goals. Their whole “reward system” is relatively flat. Life is not as much of a buzz for them as it is for most people. As with B. B. King, the thrill is gone. In fact, maybe it was never there at all.
If you have the wrong allele of the DRD2 gene, and fewer D2 receptors, and therefore you have RDS, how are you going to get the thrills those around you seem to get? Well, drugs (including alcohol), gambling, and other super-fun stuff might be the most effective way. These “rewards”  are hyper-exciting for most people. For you, who are chronically under-excited, they might be the only way to feel really engaged with life. At least until you get addicted, which seems like a step backward.
are hyper-exciting for most people. For you, who are chronically under-excited, they might be the only way to feel really engaged with life. At least until you get addicted, which seems like a step backward.
That’s the story, according to Blum. That’s what he talked about in his talk, and that’s what we argued about in the lobby for an hour. Reward deficiency leads you to seek out the biggest bang for your buck. Which makes sense, because everyone wants to feel the excitement that dopamine bestows when something special is about to happen. When I was a kid, about age eight or so, I remember making a disturbing discovery. Almost all the fun I had in life seemed to come with looking forward to things, whether a chocolate bar or a birthday present. Once the desired event was actually happening, it wasn’t as much fun anymore. (I was a weird kid, no doubt.) But for most people, a lot of pleasure comes from anticipation, from approach, and that’s what gets muted with RDS.
By the way, I’m actually working with a guy named Arnt Schellekens here in the Netherlands. He and his team are investigating low dopamine levels as a gateway to alcoholism. So this research direction is pretty close to home.
Despite its appeal, there are some serious problems with the RDS model. I’ll name just two. We know from dozens of studies that drug or alcohol use itself leads to a reduction in dopamine receptor density, or at least dopamine receptor activation, because those receptors tend to burn out or become desensitized when we keep bombarding them with fun stuff. Now that’s getting closer to B. B. King’s complaint: The thrill was there for  awhile, but now it’s gone. Sound familiar? The question remains: is your dopamine landscape more determined by your genes or by how you use them? Problem #2 is that teenagers as a group are often described in terms of reward deficiency syndrome. Teens can be seen as under-stimulated, probably because the reorganization of the nervous system in adolescence is pretty disorganized. A disorganized reorganization! That would mean that teenage thrill-seeking is not only natural, it’s inevitable, and it serves an important emotional function. Unfortunately, dangerous drugs are often part of the picnic. In other words, genetic contributions to addiction may simply be dwarfed by a tidal wave of thrill-seeking that comes with adolescence.
awhile, but now it’s gone. Sound familiar? The question remains: is your dopamine landscape more determined by your genes or by how you use them? Problem #2 is that teenagers as a group are often described in terms of reward deficiency syndrome. Teens can be seen as under-stimulated, probably because the reorganization of the nervous system in adolescence is pretty disorganized. A disorganized reorganization! That would mean that teenage thrill-seeking is not only natural, it’s inevitable, and it serves an important emotional function. Unfortunately, dangerous drugs are often part of the picnic. In other words, genetic contributions to addiction may simply be dwarfed by a tidal wave of thrill-seeking that comes with adolescence.
The jury is still out when it comes to genetic influences on addiction. Few addiction researchers doubt that such influences exist, but their exact mechanisms aren’t well understood. Blum and his colleagues are still chasing down the RDS model, and trying to connect it to other influential models, like Berridge’s incentive sensitization model. There’s a lot to be learned, and I admire researchers like Blum and Schellekens, who keep opening new doors to find out what’s behind them.