Here’s a guest post by a therapist who has been using ACT for clients with addictions for many years. Jaime highlights core principles using examples from his practice. I follow with a longish comment on aspects of ACT that I find especially important.
…by Jaime Booth Jenkins BSW MAPP…
“Between stimulus and response there is a space. In that space is our power to choose our response. In our response lies our growth and our freedom.” — Viktor E. Frankl
Acceptance and Commitment Therapy (ACT…pronounced “Act”) offers principles and techniques that can enable people to move beyond the addictive cycle…into their future. ACT arose in the ‘third wave’ of cognitive behaviour therapies and shares some fundamental principles with Dialectical Behaviour Therapy (DBT) and Mindfulness Based Cognitive Therapy (MBCT). The advantage of ACT for practitioners is the flexibility both in how it is delivered and the population it can serve. Unlike the prescriptive, manualized nature of DBT and MBCT, ACT has been shown to b e effective for both groups and individuals, for a wide range of clinical issues, and it allows the clinician to adapt core techniques as needed.
e effective for both groups and individuals, for a wide range of clinical issues, and it allows the clinician to adapt core techniques as needed.
Addiction, from an ACT perspective, is a result of experiential avoidance — the avoidance of uncomfortable and unwanted thoughts or feelings. Having a few drinks to ease social anxiety, using heroin to ease the pain of failure or trauma, or using methamphetamine to avoid boredom or loneliness are examples of experiential avoidance. Addiction adds an insidious layer of complexity because shame, guilt, self-contempt, and physiological withdrawal become feelings people also try to avoid — sometimes desperately.
ACT is based on 6 core principles:
Acceptance – Uncomfortable thoughts and feelings happen. The goal is not to avoid them, block them out, or pretend they aren’t there, but to accept them, make space for them, and then continue on. When confronting addiction there are plenty of unwanted thoughts and feelings, but one of the most challenging is CRAVING.
William was a young college student who had been using methamphetamine initially to work late — but eventually for the high itself. He had attempted to quit several times but experienced intense cravings that would lead back to using. When he experienced a craving in the session, we practiced breathing into it and visualizing himself as a surfer “surfing the wave” of discomfort. [Note the overlap with Mindfulness-Based Relapse Prevention, coming up later.] The craving dissipated and he was able to continue the session. We practiced this every time cravings arose — and eventually they became less intense.
Cognitive Defusion [sic] – Have you ever repeated a word so often that it begins to sound funny or it completely loses its meaning? This is one way to promote cognitive defusion — to remove the (fused-together) meaning or context from thoughts, words, and feelings. Defusion creates space to regard thoughts and feelings from the perspective of a dispassionate observer, making it easier to let them go and allow more beneficial thoughts and feelings to take their place.
Andy was a high-powered lawyer with a cocaine addiction. He had an extreme reaction to the word “addict” and would go to great lengths to avoid labeling himself that way. The shame of the word itself increased his desire to use. To take the power out of the word we practiced a few different defusion techniques. Changing the words of Happy Birthday to “Happy Addict,” imaging a baby elephant saying the word or repeating it over and over in different tones and voices, it began to lose its meaning and therefore its power.
 Being Present – Staying present in the face of uncomfortable internal or external stimuli, without judgement, can be difficult when coming out of an addiction. Painful thoughts and feelings can return without warning and overwhelm the individual.
Being Present – Staying present in the face of uncomfortable internal or external stimuli, without judgement, can be difficult when coming out of an addiction. Painful thoughts and feelings can return without warning and overwhelm the individual.
Every client I see is given a pack of Lifesaver candies (sweet little O’s, multi-coloured, etc). We then run through a simple “lifesaving” meditation in order to practice remaining in the present. Putting a candy in your mouth and focusing on what it looks like, tastes like and feels like allows you to return to the present. If a particularly painful rumination begins, pulling out a lifesaver is a quick and easy way to return to what’s actually happening in the present. Other therapists use other techniques to snap the client out of the “monkey chatter” of cycling thoughts and into the here-and-now.
The Observing Self – This is perhaps where Frankl’s space becomes the most literal, as it requires individuals to distance themselves from their thoughts and feelings and observe them as if they were a separate entity. Having these thoughts and feelings is normal, but this doesn’t make them valid or true.
Emily struggled with the shame associated with some of her actions while drunk. Self-deprecating thoughts about these actions would scream at her and pull her back into drinking. In order to help her regain control we 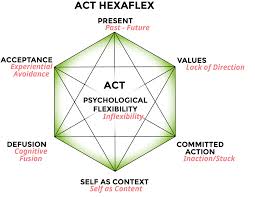 practiced a mindfulness activity in which she was laying on the ground and watching her thoughts float by like clouds. She simply watched, without judging or avoiding. This gave her the opportunity to see her thoughts as separate from herself, and gave her the space to decide whether to grab the thought or let it pass by.
practiced a mindfulness activity in which she was laying on the ground and watching her thoughts float by like clouds. She simply watched, without judging or avoiding. This gave her the opportunity to see her thoughts as separate from herself, and gave her the space to decide whether to grab the thought or let it pass by.
Values – It is not uncommon for an addiction to become the central unifying purpose of an individual’s life. This tends to obscure what is of real importance.
Claire was in my office because her employer noticed her showing up late for work, taking more breaks throughout the day, and taking more “sick days” than others in her position. She revealed to HR that she regularly drank 1-2 bottles of wine each evening and did not see a reason to stop as she was near retirement. It was not until we came to identify her core values — connecting closely with family and friends — that she was able to see the  real impact of her addiction: it was pulling her farther away from them. So now, when she would experience a craving in the session, instead of focusing on not drinking, we would choose an image of interacting with her children as a focal point to move towards. Her value acted as a lighthouse that guided her through the craving. She was willing to experience the discomfort of craving because she knew, on the other side of it, her family was waiting, and she wanted that more than she wanted to avoid the discomfort.
real impact of her addiction: it was pulling her farther away from them. So now, when she would experience a craving in the session, instead of focusing on not drinking, we would choose an image of interacting with her children as a focal point to move towards. Her value acted as a lighthouse that guided her through the craving. She was willing to experience the discomfort of craving because she knew, on the other side of it, her family was waiting, and she wanted that more than she wanted to avoid the discomfort.
Committed Action – Once a space has been created and values identified we can begin to allow ourselves to be pulled by our future instead of pushed by our past.
Continuing work with Claire involved helping her to set goals that would allow her to live a life more aligned with her values. We set the goal of having interactions with her family or making plans with a friend without wine. Simple — and she much preferred how it felt, once she got used to it.
A silver bullet to “solve” addiction is something I have been searching for throughout my career. But there are likely as many silver bullets as there are individuals. What I have found in ACT is a framework that allows people to regain control, not over their addiction but over their thoughts, feelings, and actions. This control allows them to move in value-led directions — and their addiction can dissipate as a by-product. The work to get there is not easy — but it is certainly worth it.
Helpful Links:
Training/books by Russell Harris, an ACT-based practitioner/trainer.
Detailed outline of ACT, principles and practice, also by Russ Harris, from Psychotherapy.net.
Summary and links, Association for Contextual Behavioral Science.
Urge surfing…wrt addiction. From “Mindfulness with Dr. Walsh,” 2016.
Great interview (video) with Steven Hayes, by “Dr. Dave — The Science of Psychotherapy,” 2019.
 genius. He was the first (as far as I know) to develop a “talking cure” for serious emotional difficulties, and he was the first to bring the idea of unconscious wishes and motives into public parlance. Sure,
genius. He was the first (as far as I know) to develop a “talking cure” for serious emotional difficulties, and he was the first to bring the idea of unconscious wishes and motives into public parlance. Sure,  psychoanalysis — on the couch, four times a week, for fifteen years (?!) — hasn’t lived up to expectations, and I believe it’s correctly pushed aside by more focused, present-tense-oriented, and evidence-based treatment models.
psychoanalysis — on the couch, four times a week, for fifteen years (?!) — hasn’t lived up to expectations, and I believe it’s correctly pushed aside by more focused, present-tense-oriented, and evidence-based treatment models. with a capital S is to be our lodestone, then psychoanalysis doesn’t look so hot either. But, okay, Dodes is inspiring, he’s developed his methods over decades, he’s come
with a capital S is to be our lodestone, then psychoanalysis doesn’t look so hot either. But, okay, Dodes is inspiring, he’s developed his methods over decades, he’s come  problems in the light of one’s early development. A realistic and increasingly popular spin-off of this position is the emphasis on childhood trauma, most famously highlighted by
problems in the light of one’s early development. A realistic and increasingly popular spin-off of this position is the emphasis on childhood trauma, most famously highlighted by  There are addiction treatment centres (e.g.,
There are addiction treatment centres (e.g.,  offers a harm-reduction approach that has psychodynamic psychology (and thus individual psychotherapy) built into it. I particularly like Tatarsky’s model (I spoke there and met him last June) because it is fundamentally empathic and humanistic, honouring individual differences and working with them.
offers a harm-reduction approach that has psychodynamic psychology (and thus individual psychotherapy) built into it. I particularly like Tatarsky’s model (I spoke there and met him last June) because it is fundamentally empathic and humanistic, honouring individual differences and working with them. What’s most interesting to me is how psychodynamic ideas provide a foundation underlying many current schools of psychotherapy. With respect to addiction, ACT and IFS (my favourites — see last post) are all about bringing the past into the present and dealing with it. What seems to be missing from our lives? When did that start? Where does the depression come from? What messages do we repeatedly give ourselves that make us feel hopeless or despicable, so there seems little opportunity for relief except our addiction? Where do contradictory self-statements, like yes, this is what I want and I hate doing this! actually come from?
What’s most interesting to me is how psychodynamic ideas provide a foundation underlying many current schools of psychotherapy. With respect to addiction, ACT and IFS (my favourites — see last post) are all about bringing the past into the present and dealing with it. What seems to be missing from our lives? When did that start? Where does the depression come from? What messages do we repeatedly give ourselves that make us feel hopeless or despicable, so there seems little opportunity for relief except our addiction? Where do contradictory self-statements, like yes, this is what I want and I hate doing this! actually come from? psychotherapists do, is blend different approaches, revising and refining our methods until we find what works best. And what works best appears at the interface of our own personality and knowledge base, our style of connecting with others, and the particular problems (in my case, mostly addiction) that come our way.
psychotherapists do, is blend different approaches, revising and refining our methods until we find what works best. And what works best appears at the interface of our own personality and knowledge base, our style of connecting with others, and the particular problems (in my case, mostly addiction) that come our way.
 themselves, sometimes despite vast challenges (including abuse of one kind or another) during childhood and/or adolescence. And I’ve helped people devise cognitive tricks to shunt their trajectory away from substance use and toward more satisfying habits.
themselves, sometimes despite vast challenges (including abuse of one kind or another) during childhood and/or adolescence. And I’ve helped people devise cognitive tricks to shunt their trajectory away from substance use and toward more satisfying habits. But there seems to be a black hole in the centre of the addiction galaxy that sucks in techniques of every sort and laughingly squishes them to nothing, tosses them back down some wormhole to some parallel universe. And surely that’s because addiction boils down to a unique “thing” which is totally psychological, totally biological, and totally social. A habit in the workings of our cells, our minds, and our interpersonal relations.
But there seems to be a black hole in the centre of the addiction galaxy that sucks in techniques of every sort and laughingly squishes them to nothing, tosses them back down some wormhole to some parallel universe. And surely that’s because addiction boils down to a unique “thing” which is totally psychological, totally biological, and totally social. A habit in the workings of our cells, our minds, and our interpersonal relations. later) you’re often left with an aching emptiness. And what the hell are we humans supposed to do with that?! (Mindfulness/meditation has some answers, but let’s face it, the solution isn’t obvious.)
later) you’re often left with an aching emptiness. And what the hell are we humans supposed to do with that?! (Mindfulness/meditation has some answers, but let’s face it, the solution isn’t obvious.)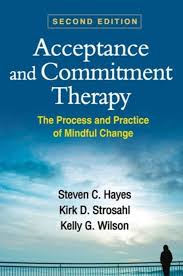
 IFS
IFS
 Though outwardly I was the soul of enthusiastic compliance with my treatment, the questions were brewing. I didn’t think that character defects and self-centeredness had caused my alcohol problems. I had no interest in spending my life confessing my sins to strangers. And I wasn’t convinced that a lifelong abstinence from any mood-altering chemical (except caffeine, sugar and nicotine!) was the only answer.
Though outwardly I was the soul of enthusiastic compliance with my treatment, the questions were brewing. I didn’t think that character defects and self-centeredness had caused my alcohol problems. I had no interest in spending my life confessing my sins to strangers. And I wasn’t convinced that a lifelong abstinence from any mood-altering chemical (except caffeine, sugar and nicotine!) was the only answer. We don’t require anything, other than that members treat each other with respect and not judgement. We support abstinence (a word we prefer over “sobriety,” as “sober” has moral connotations), moderate drinking, and safe drinking.
We don’t require anything, other than that members treat each other with respect and not judgement. We support abstinence (a word we prefer over “sobriety,” as “sober” has moral connotations), moderate drinking, and safe drinking. For me, HAMS has been a critical part of rewriting my identity. The label “alcoholic” seemed to erase everything I had been before, and everything I might be in the future. No matter what I did, even when I didn’t drink, I felt shame. HAMS has taught me that the content of my bloodstream is not the content of my character. Now my identity is not defined by my relationship to alcohol. I am not an “alcoholic.” I am April Wilson Smith.
For me, HAMS has been a critical part of rewriting my identity. The label “alcoholic” seemed to erase everything I had been before, and everything I might be in the future. No matter what I did, even when I didn’t drink, I felt shame. HAMS has taught me that the content of my bloodstream is not the content of my character. Now my identity is not defined by my relationship to alcohol. I am not an “alcoholic.” I am April Wilson Smith. HAMS has just published
HAMS has just published 
 attractive (and challenging!) to today’s intrepid psychonaut. And by the way,
attractive (and challenging!) to today’s intrepid psychonaut. And by the way,  There’s much to say about the ritualistic use of DMT by aboriginal cultures, the shamanic element, the social contexts considered helpful and supportive, and the limited research conducted so far.
There’s much to say about the ritualistic use of DMT by aboriginal cultures, the shamanic element, the social contexts considered helpful and supportive, and the limited research conducted so far.  More recently, I heard an intriguing description of a trip with The Toad.
More recently, I heard an intriguing description of a trip with The Toad.  afraid of this moment for days. My friend spoke about “ego death” — leaving your personality behind, essentially dying as an individual and becoming connected with the rest of the universe intimately but without control. Sure, I was scared. “Ego death” has the word “death” in it.
afraid of this moment for days. My friend spoke about “ego death” — leaving your personality behind, essentially dying as an individual and becoming connected with the rest of the universe intimately but without control. Sure, I was scared. “Ego death” has the word “death” in it. lungs would burst. And then the room began to dissolve before my eyes. All of its features simply faded to colourful outlines and then…nothing at all. Strong hands helped me to lie back. Close your eyes now — I could still hear his voice. But I wasn’t in the room anymore.
lungs would burst. And then the room began to dissolve before my eyes. All of its features simply faded to colourful outlines and then…nothing at all. Strong hands helped me to lie back. Close your eyes now — I could still hear his voice. But I wasn’t in the room anymore.