…by Colin Brewer…
 Last post I suggested that we can attend to (rather than reject) our cravings and pursue integration rather than abstinence. Today, a contrasting view: Colin Brewer, a renowned and controversial addiction doctor, explains how Antabuse and naltrexone can free us from endless ruminations while new habits take root and grow.
Last post I suggested that we can attend to (rather than reject) our cravings and pursue integration rather than abstinence. Today, a contrasting view: Colin Brewer, a renowned and controversial addiction doctor, explains how Antabuse and naltrexone can free us from endless ruminations while new habits take root and grow.
………………………………
Having plenty of spare time on Covid lockdown, can I float a couple of evidence-based ideas to this experienced readership? (My own experience is only as a physician who treated assorted addicts. Unlike many US addiction medics, most European ones are not ‘in recovery’.)
1. Though not all substance abuse represents the drowning of internal and external sorrows, quite a lot does. However, the main difference between those who drown them and those who don’t is not that the former have bigger sorrows to drown; it’s that they have got into the habit of drowning them while the others have not. Addiction is therefore to a large extent a matter of habit and habits can be unlearned as well as learned. One of our main habits is speaking only one language. To learn another language requires the unlearning of that habit for long enough to allow another linguistic habit to get established. Research — lots of it — consistently shows that the best and quickest way to learn a new language and become fluent is to be forced to speak the new language exclusively from Day 1 for hours at a time, however badly. Language schools charge big fees for creating an environment where this happens and students routinely achieve at least basic fluency within a week. You can do the same by living on your own in a village where nobody speaks English. Necessity is a great teacher.
2. In the case of drug addiction (including alcohol of course) the evidence strongly indicates — as does common sense — that people who have not responded well to previous treatment and have had several relapses with no more than a few weeks or months of abstinence, need at least 18 months of 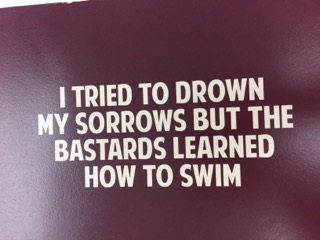 abstinence before they change their self-image from “I’m an addict/in recovery” to “I used to be an addict but now I’m different.” Keeping these treatment-resistant addicts drug-free — or at least free of their main problem drug — for 18-24 months is made a lot easier by the consistent use of drugs that deter their use. Disulfiram (Antabuse) deters alcohol use by the prospect of an unpleasant physical reaction and naltrexone deters opiate use by the prospect of an unpleasant psychological reaction.
abstinence before they change their self-image from “I’m an addict/in recovery” to “I used to be an addict but now I’m different.” Keeping these treatment-resistant addicts drug-free — or at least free of their main problem drug — for 18-24 months is made a lot easier by the consistent use of drugs that deter their use. Disulfiram (Antabuse) deters alcohol use by the prospect of an unpleasant physical reaction and naltrexone deters opiate use by the prospect of an unpleasant psychological reaction.
The German OLITA study — probably the most important (and encouraging) alcoholism treatment study bar none — showed that once a group of very unpromising alcoholics with numerous treatment failures had taken disulfiram 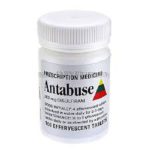 under supervision (and thus stayed dry) for at least 20 months,
under supervision (and thus stayed dry) for at least 20 months,  most of them stayed dry without disulfiram (and mostly without other treatment) for the next 7 years of follow-up. In other words, by simple daily practice and repetition, their alcohol-using habits had been abandoned and replaced by habits that didn’t include alcohol. We don’t yet have similar long-term studies of naltrexone for opiate dependence but with naltrexone implants that can last six-months or even a year
most of them stayed dry without disulfiram (and mostly without other treatment) for the next 7 years of follow-up. In other words, by simple daily practice and repetition, their alcohol-using habits had been abandoned and replaced by habits that didn’t include alcohol. We don’t yet have similar long-term studies of naltrexone for opiate dependence but with naltrexone implants that can last six-months or even a year  in existence or in development, we soon will have. I predict that the longer-acting the implant, the better the results will be because fewer decisions to continue treatment (compared with monthly Vivitrol injections) need to be made in the crucial first few months.
in existence or in development, we soon will have. I predict that the longer-acting the implant, the better the results will be because fewer decisions to continue treatment (compared with monthly Vivitrol injections) need to be made in the crucial first few months.
A recent New Zealand study showed how disulfiram effectively removes one of the most annoying features of being an alcoholic — the endless internal arguments and conversations that patients have with themselves almost every minute of the day about whether they should or shouldn’t drink. Some patients described it as a sort of “internal homunculus that demanded alcohol.” Disulfiram replaced those endless ruminations and temptations with a mind-set in which alcohol was “simply no longer an option.” One patient described how, when he wasn’t taking disulfiram, after all the internal arguments, “at the end of it, I just go ‘fuck it, fuck it’… When I’m on Antabuse, it’s just like. Well, I can’t.” After a year or even less, that ‘Well, I can’t’ increasingly morphs into ‘Well, it doesn’t seem that important now. I’m learning to manage without it and I’ve found other things to do instead.’
Some people who have learned to become indifferent to alcohol can even progress to cautious experiments with controlled drinking, though if it gets uncontrolled, they should get the message and not try again. And I doubt whether trying controlled opiate use is ever a good idea. However, there are undoubtedly people whose brains do not adapt to long-term opiate abstinence and who are better off on long-term methadone, buprenorphine or — in Britain at least — morphine.
I’d really appreciate the views of people for whom those internal arguments are a daily experience — or were until recently; or who have left them behind. I am fortunate only to have encountered them at second hand.
…………..
Brewer C, Streel E. Antabuse treatment for alcoholism. An evidence-based handbook for medical and non-medical clinicians. Foreword by William R Miller. CreateSpace IPP. North Charleston, SC. 2018
 Informed by unparalleled neuroscientific insight and written with his usual flare, Marc Lewis’s The Biology of Desire effectively refutes the medical view of addiction as a brain disease. A bracing and informative corrective to the muddle that now characterizes public and professional discourse on this topic.” —Gabor Maté, M.D., author of In The Realm of Hungry Ghosts: Close Encounters With Addiction
Informed by unparalleled neuroscientific insight and written with his usual flare, Marc Lewis’s The Biology of Desire effectively refutes the medical view of addiction as a brain disease. A bracing and informative corrective to the muddle that now characterizes public and professional discourse on this topic.” —Gabor Maté, M.D., author of In The Realm of Hungry Ghosts: Close Encounters With Addiction
Great post, as recovering/addict near a point of the “can say I am a different person now” (6 months). Amphetamine was my vice, be it in the form of “speed” or the more potent methamphetamine variety. This was my near 3 times weekly habit from around 18years old till around 31 years old.
I had begun to sense something more than the habit of using these drugs was because of my depression and anxiety when my partner let me try their concerta ADHD medication and like night and day my craving for anything amphetamine based had subsided and I was able to fill the void that it had been filling.
After clinical diagnosis with ADHD, I after numerous trials of concerta, vyvanse and ritalin found dexamphetamine (Adderall) was most effective. It took quite a while to adjust with maintenance of proper use of dex, but it was the most successful addition to my life that helped me “ween” off using street amphetamine products.
As I am now a 2nd year Psych and Counseling major with addition to wanting to better understand my own self, I’ve done a bunch of research into different studies surrounding addiction for drugs like cocaine, heroin, speed etc. and have come to the position that it will either be a combination of both a medical and therapeutic intervention to overcome addition for some and others will not need the medical aspect e.g. medication.
I feel the 18 month time frame is a really good approximation in how long it can take to reach a place where one does not think about the drug of choice in the same way, and, with the right intervention for the right person after 3 months – atleast in my personal experience, begin to see the benifits vs the cost starts to be weighed more strongly on the cessation of substance abuse.
Thanks for sharing this, Alejandro. It is interesting — isn’t it? — that these psychological processes, including the time frame of a modified emotional response, cross over from one substance to another. But I think the time it takes to stop craving something can be broken down into smaller phases when we put context into the equation. I remember it was about 3 months since I quit opiates, back in my mid-twenties, when I truly didn’t think about it, except, one fateful (for me) night, at a party, after a couple of drinks, standing in front of the host’s medicine chest. Then…all was lost for another year or two.
Context-based sensitivity translates into “how safe am I?” in situation x, y or z? And for me (and others) x, y, and z can be very difficult to pinpoint and predict in advance. Seems to me that that’s a solid argument for long-term use of substances like naltrexone and disulfiram. You don’t really know how “safe” you are, from one context to another…for quite some time.
Hi Marc,
Thanks for your reply, this and your previous posts, blogs, guest spots, YouTube talks (and of course you’re books) are a constant motivation for me in my own personal form of “recovery” and further academic studies.
Looking at an equation that informs an individuals context-based sensitivity is not an area of thought that I had not come across before. But I love!
Research into a similar questions, that I have come across will more broadly study the identification of umbrella terms such as “triggers” for population generalisability which atleast for me makes sense at the present time.
I would love to study the use of a model; using an equation to accurately determine individual context-based sensitivity. If I was able to complete such a study that has this outcome allowing to target and inform treatment interventions (medical, therapeutic, etc) for specific individuals would be quite a revolution.
I guess, limitations of my research validity (as you mentioned, the difficulty to predict situations in advance) could only be accurate when I have a flux capacitor fitted into a Delorean 😅.
So then that opens up the one of many time travel paradox’s, such as, the very fact of knowing your own future will inherently change that future the moment you become consciously aware. Thus, a situation of substance resuse is newly created in time and space that never would have happened (previous to that future knowledge) will now happen. 🤯
If I understand you, then we agree that contexts don’t come in categories — at least not predefined categories. Hence there’s no basis for predicting context-specific outcomes. That’s why things like average time spans often mean very little when thinking about the individual.
And thanks for letting me know that my blathering has been of use!
Hi Marc,
Yep, spot on.
Looking forward to your future posts, insights, discussions etc.
P.S, on an unrelated topic, a previous blog where you used an example of crossing the road on a red light vs. not, thus, those that are watching others cross whilst undergoing their own personal existential crisis (me – haha) has made a significant difference in how i notice and process my thoughts for both similar and opposite moments in time with more clarity and mindfulness.
Hope you stay safe and healthy with all that is currently happening around.
Cheers,
Alex
Hi Marc. Just testing as requested to see if my lost replies reach you from another computer.
Makes sense what works works what doesn’t doesn’t. Rumination’s and fixations are painful and can seem never ending but eventually they do simmer down and often simply almost entirely go away. I guess what about multi or poly addictions? However I get the point and habits can be unlearned but it’s not easy and the remnants of the pathways still fire and shout even after decades regardless of the other changes, healing or transformations that have come to fruition. Change is hard worn and fir some there are no easier routes but I get the points being made.
Warmest Regards
CM
Thanks for this post Colin. Just wondering if you’ve heard of the Sinclair Method, as a way of supporting alcohol cessation, and, if so, what are your views on it? I’m currently working with a client who really fits in with holding on to one deeply entrenched language and fantasy about his relationship with alcohol. I have been involved with him, as his counselor, for the past six weeks. During that time he has managed just over three weeks abstinence, two when I first met him and for the past week. For the past few days he’s literally been hanging on to the cliff edge, staying sober for everyone except himself. We agreed, only this morning, that he can realistically manage only one more week sober and I am trying to work out the best way forward. Along with his consultant psychiatrist, we are looking at changing his antidepressant over the next few days. For me the options are;
1. Introduce disulfiram or naltrexone as a relapse preventative. More or less as you describe here.
2. Introduce naltrexone as per the Sinclair Method and support him whilst he reestablishes his relationship with alcohol.
I am also a mental health nurse and have used both methods, many times, with success prior to this. However I have found that, for the profile of this particular guy, the Sinclair Method has been much more successful.
I would be interested to get some feedback from yourself and the rest of the community.
Many thanks
Peter
Hiya Marc
Hope you’re well and surviving the crisis
Hello Peter. The Sinclair method has been heavily hyped (not least by its founder) but compared with placebo, naltrexone (NTX) actually has very modest specific effects on alcohol consumption (as opposed to its much higher effectiveness in opiate abuse). The placebo effect of many medications – which is also a component of the overall effectiveness of active medicines – is considerable and widely under-rated. There are several negative or very marginally positive trials of NTX in alcoholism, including some of depot NTX where compliance was not a factor but there are no negative trials of properly supervised DSF. However, as Marilyn Skinner in particular has pointed out, the similar deterrent effect of placebo DSF in blind placebo-controlled trials means that uniquely for medication studies, this sort of trial is unsuited to DSF. TSM is supposed to help people drink less rather than abstain, though some NTX clinical trials used abstinence rather than reduction as the main endpoint. If your patient insists on aiming at controlled drinking, you might be able to persuade him that his chances of success (which seem modest from your description) would be higher if he were to try it after a minimum of 3 months of abstinence – or twice his previous record, whichever is the longer. If that fails, he should review his choices after 18 abstinent months. Either way, DSF – supervised by family and/or treatment team – will make it easier for him to abstain for that period. Even three months of abstinence will also make it much easier to decide whether he has ‘depression’ as opposed to ‘understandable unhappiness’ because of his alcohol problem and its likely effects on many aspects of his life and relationships. ‘Depression’ often disappears or becomes very manageable without medication when that happens.
Please let me know how things develop.
Colin
A discussion of disulfiram’s considerably greater effectiveness compared with naltrexone or acamprosate, as well as other aspects of disulfiram treatment and its history, can be found in my book. Please see publication details at the bottom of the main post.
Hi Peter,
Always a pleasure to see you here, and I’m glad Colin replied directly and thoroughly. Seems that everything revolves around the person’s willingness to try abstinence, even briefly, before moving onto controlled use. I’ve learned that some of my clients really can’t stay completely “off” for more than a few days at a time. So be it. So then we set up a schedule. Even one day “off” between “on” days can be hugely valuable. It’s the beginning of learning that there are joys that don’t hinge on use of the substance. And then, we can either extend the “off” times or else start right in building limits for the “on” times (plus other helpful cognitive “tricks” — like making sure there’s only a certain amount available at a time). It all depends on the individual, as you and I know well.
Hi Colin, A couple of thoughts to share: I am a social worker/therapist in her late 60s who has been an addict on and off since adolescence. My drug(s) of choice were in the depressant category, including alcohol, barbiturates, valium, and opiates. I have managed to live a relatively normal life despite addictions. During a particularly stressful period in my life, starting 25 years ago, I became addicted to prescription opiates. As a result I’ve been on a generic version of Suboxone for the last 15 years. The addiction doctor I originally started with felt I should continue on it as it also worked as an anti-depressant. What I’ve found over these years on Suboxone is that I have never been rid of cravings to “get high.” What happens is that being on Suboxone creates a stability of sorts, leaving the issue of what do I do when I’ve had a particularly trying day? Nothing that involves a substance. I, like so many unaddicted people, was used to (during sober times) having a glass of wine just to “chill out” but Suboxone distorts the effect of alcohol, making a glass of wine ineffective as a relaxant and marginally unpleasant. As a therapist and in therapy myself I knew that there are other, non-substance ways of addressing stress, such as exercise, meditation, etc. But to be honest, I never got fully away from wanting instant relaxation, the kind that a drink, pill or powder gives. Fortunately though, the Suboxone made turning to one of these impossible. So I’ve stayed on it. I’ve also identified in myself the need on a daily basis to “take something.” It was/is the behavior I’ve been in the habit of doing. So I’ve been “taking” Suboxone, satisfying the need to take something. Finally, I’ve turned to other, behavioral addictions such as shopping. Nothing like whiling away the hours, lost in a website that sells beautiful clothes, jewelry, art, etc. This habit has caused me to have debt I shouldn’t have. I’ve often wanted to try and get off Suboxone and quickly realized doing so might be asking for trouble. So I stay on it and grapple with my cravings and behavioral addictions. Both of these are manageable and not irrevocably damaging. And really finally, reading the analogy of learning a foreign language by being immersed for a week in a setting in which one has to speak the language… the language gets learned by necessity during the class but isn’t it just like getting sober during detox, then returning to one’s usual environment where one loses the sobriety, or, in the analogy, the language. I say this as a comparison to my lifelong cravings, even as I’ve been “clean” for 15 years. Thanks for your work!
Thanks Denise. I tried to reply a few days ago but it disappeared into cyberspace. What you describe sounds like ‘harm reduction’ that has reduced a number of harms as well as drug misuse. Many patients, doctors and therapists are happy with that provided that the reduction is significant and allows some sort of reasonably, normal, acceptable or gainful existence, as yours seems to have been. It’s interesting that suboxone blunts your response to other drugs. Some people might point to the similarity of the naloxone component of suboxone to naltrexone and argue that it supports the idea of naltrexone as a generalised anti-craving drug but the naloxone is hardly absorbed unless suboxone is injected, so if it is a true drug effect, it would be the buprenorphine component. That makes sense because in some people, opiates do have both mood altering and mood stabilising effects and there are case reports and some clinical trials indicating useful effects in some cases of resistant depression.
I agree with you that not everybody gets used to abstinence, even with medication-assisted practice and as your your own account shows, not everybody manages to leave cravings behind. However, as long as the cravings are generally resisted, or converted into cravings that are less damaging, that’s still progress. In my experience, people who have got as far as you have in life – in both senses – are not at high risk of major relapses.
The great advantage of Antabuse and naltrexone is that after detox (the easy bit) they do make it much easier to return to your normal environment and get used to walking past rather than into the local bottle-shops or dealers at a time when the risk of relapse is otherwise extremely high.
While I can identify with the arguments that people whose goal is abstinence or who are trapped in “recovery” thinking (I’ll always be an addict/alcoholic, this is my identity and I am doomed), I think this approach has some serious problems.
As someone who suffers from severe PTSD, including paralyzing panic attacks that have led to self-harm in the past, drugs that bring on serious physical and psychological reactions (to call them “unpleasant” is a vast understatement, based on the experience of people I know who’ve taken Antabuse, as well as the advisement of the clinical psychologist who said she would not treat me if I refused to take Antabuse), could cause life-threatening reactivation of panic and PTSD.
Also, these approaches are essentially punitive. They do nothing to relieve the underlying causes of most addiction: depression, trauma, anxiety, etc.), and leave the person suffering with simply the absence of a coping mechanism, not a new coping mechanism. It’s all well and good to say, “Well, just develop new coping mechanisms,” but those of us who have to work almost all the time just to make ends meet and are under real threat of domestic violence, gang violence, being locked up for not being white, etc., don’t have time to engage in the typically suggested practices of meditation, yoga, extensive and expensive therapy (and most good psychiatrists and therapists don’t take insurance, certainly not Medicaid. They also come from backgrounds that make it difficult for them to understand the struggles of those of us who aren’t well-off. My deepest respect to the social workers who refuse to work in offices filled with table fountains and green tea and instead provide their clients with granola bars and sanitary supplies and bus tokens.)
Substance use definitely usually doesn’t help any of these situations, but just abstinence won’t either. In fact, a plunge into abstinence without social and economic support could plunge a person into even more dangerous behavior.
Medications such as baclofen, the little known in the US but common in Europe medication that treats alcohol cravings, anxiety and PTSD (see my article on it here: https://www.rehabs.com/pro-talk/the-truth-about-taking-high-doses-of-baclofen-to-suppress-alcohol-cravings/) treat the causes of substance use, and do not create severe punishments for those who slip up. Even the vilified benzos, in safe and medically monitored doses by psychiatrists who know what they’re doing, greatly help anxiety and panic disorders and are a whole lot better than binge drinking or other chaotic substance use.
As is so common for traditional, top-down, goals set by the professionals instead of by the people treatment styles, this post sets the only goal as abstinence. Like many of my intellectual forefathers and foremothers: Stanton Peele, Kenneth Anderson, Patt Denning and Jeannie Little to name just a few, the goal should be a happy, fulfilling life, as defined by the individual. If abstinence facilitates that, great. But abstinence is not the only definition of success.
That’s why I am committed to HAMS (Harm Reduction, Abstinence and Moderation Support), a non-judgmental, worldwide support group that encourages individuals to set their own goals and provides tools and support to achieve those goals. Please see my recent post if interested.
Thanks April. I’ll reply to some of your points in more detail when more responses are in. For the moment, I just want to make it clear that – as I hope is obvious since I’m not opposed to controlled drinking – I don’t regard abstinence as the only acceptable goal and would always offer patients a treatment menu. I also mentioned that some patients never adapt to abstinence from opiates and may do better on indefinite opiate maintenance. I’m keen on naltrexone but I think I hold the UK record for methadone maintenance dose – a professional with a strong needle habit who continued working on a dose of 1000mg oral and 100mg i/v daily.
April, please see my reply to Terry below. It’s meant for both of you. I think you bring up many valid points. People need help in all kinds of ways. But that doesn’t add up to rejecting one approach because it doesn’t incorporate half a dozen other elements that can also be beneficial.
Damn, I was near done with a co.ment and hit something and it’s gone. See, I screw everything up.Technology is not my friend. I run to Meth. My form of addiction is escape. I was a RN11 yrs. Until 2007. Gave it to crack then. Felon. No jobs I can do. Low self esteem. Nervous in social setting. No patience. Frustrated . I’ve had periods of stopping. 1- 3 months. Not into the AAs. I use maybe 3 days per week. So, say $60. I have no income. Me sober boyfriend gives me a little money each week. Ok that’s all. It sucks but my brain wont let go.
both those drugs have been around for a long time – and little has changed – what would make ‘addicts’ want to take them for such along period of time when so far drop outs account for most failures using those medications. In the case of Antabuse a drinker only has to decide not to take it and away they go,again. And as April says this assumes the goal of any addict is to be abstinent but if abstinence is just that, no use, and nothing else of meaning is in the persons life then their abstinence will be achieved with misery as a companion. A ‘dry’ drunk as they say can be a sad sight. Again this answer lies in the absence of the drug, something prohibitionist have been espousing for years now to little effect, yet stress in individuals is increasing at dire rates, especially now. How many addicts will be produced in response to this virus ? yet that would have nothing to do with the direct action of the drug (drugs aren’t viruses – ya can’t catch addiction) rather the fear and stress pervading peoples very being and the helplessness and hopelessness of loosing a job and seeing all sense of meaning and achievement lost in a flash …
Terry, April, I don’t see why you infer that Colin is claiming that abstinence is the only way. As he notes above, his post provides concrete examples of non-abstinent outcomes that work well for many people. I don’t read his post as insisting on one approach for all. It’s one way. And for many people it’s the preferred way, though, as I set out in my last post, non-abstinence can be valid and beneficial too.
A consensus often reached by this community is that different people have vastly different preferences and needs, and help or treatment should be sensitive to those differences.
Once you acknowledge that some people really will do better with total abstinence, I see disulfiram and naltrexone simply as scaffolds or supports that are most effective if taken over prolonged periods early in recovery. I just don’t see a problem with that. Many people ask me whether they should take antidepressants, and (despite low effectiveness demonstrated by several meta-analyses) I don’t see a problem with that either, though I advise it as an adjunct to psychological work and/or mindfulness/meditation. Again as a bridge or scaffold during a difficult period or a period of transition. Hell, ride on the placebo effect for that matter. Or buy a pet poodle if that helps.
Don’t most of us agree with the “whatever works” policy?
Hi Terry and Marc,
I agree with “whatever works.” I often say, “Hey, if throwing spaghetti against a wall works, go ahead and do it!” Though if it’s covered in marinara, please don’t throw it against my wall!
Hi Terry,
I’ve been thinking a lot about the point you raise – addiction being fueled by this crisis. That’s why I wrote, with Kenneth Anderson, my most recent article in Filter, “Safer Drinking in Desperate Times” https://filtermag.org/safer-drinking-coronavirus.
I completely agree that for many, few life goals can be accomplished without abstinence. I disagree, however, that addiction is not contagious. Living in a community where addiction or heavy use is more socially acceptable does raise one’s chances of addiction, just like a virus: Study Says Obesity Can Be Contagious: https://www.nytimes.com/2007/07/25/health/25cnd-fat.html in the New York Times discusses this, as does an excellent TED talk by Nicholas Christikas, https://www.ted.com/talks/nicholas_christakis_the_hidden_influence_of_social_networks/transcript?language=en. Heavy drinkers tend to hang out with other heavy drinkers, many of whom are addicted. Virtual happy hours are popping up online as people drink away the misery.
How can we make substance use that is not problematic (including abstinence) contagious too?
Hi – well i mentioned contagious from a purely medical type point of view – you can’t stand within 1.5 meters of an alcoholic for a short time and catch alcoholism but i totally agree that living in and around users increases risk of using and thus risk of addiction (in a small percentage of those users) – as does belonging to certain cultural groups many of whom are disconnected or traumatized. What i am saying is that we typically emphasis the action of the drug rather than the ‘set and setting’ and for sure now those factors are changing for people. How many more will now be lonely, especially the elderly, how many helpless and hopeless without work, how many in chronic fear of catching this thing or of being unable to feed themselves or their families – anxiety is one the rise and anxiety fuels addiction – of course many are already up and running with internet, gaming and social media use skyrocketing as the deliberately created cyber addictions come into their own and reach peaks at this time. But like drugs the connections social media affords are not as real nor ultimately satisfying as face to face connection and are often the arena for trolls and abuse, faceless judgement and scorn. My sadness is that my gym addiction cannot occur as it did but as any intrepid addict can do i have made my own gym on my back veranda and carry on the cause, but i fear that for many alcoholics and drug dependent people this will be a very hard time, in part because many are unhealthy, homeless and often in withdrawal, prime candidates for a virus – non problematic substance use is made contagious by one source – the media and advertising that affects public opinion and makes certain drugs socially acceptable – in Australia the addiction still raging on is gambling as horse racing is about the only ‘sport’ remaining active.
Apologies for the delay in responding. There have been some technical problems. You ask – quite reasonably – ” what would make ‘addicts’ want to take [Antabuse] for such a long period of time when so far drop outs account for most failures using those medications. In the case of Antabuse a drinker only has to decide not to take it and away they go,again.” That is true for people who are just given a bottle of tablets and asked to take them daily. It is not true for the only sensible and evidence-based way of prescribing Antabuse, which is to involve a third party in supervising it. I strongly urge anyone who doubts that to read the OLITA study I mentioned.(Krampe H, Stawicki S, Wagner T, Bartels C, Aust C, Rüther E, Poser
W, Ehrenreich H. Follow-up of 180 alcoholic patients for up to 7 years
after outpatient treatment: impact of alcohol deterrents on outcome. Alc
Clin Exp Res. 2006; 30(1):86-95.)
Despite being a group of patients with many treatment failures and high alcohol intake (over a bottle of spirits daily) the outcomes at 9 yrs were very good.
Hello, I am delighted to see a post by Colin on ‘abstinence’, perhaps the most controversial noun in our field! By way of introduction, I worked for the pharma company that developed naltrexone and my job many moons ago was to train physicians how use this medication. I left the company almost 21 years ago to start evidence-based medical treatment for addictive disorders. In the 21 years of existence my clinics have treated in excess of 16,000 patients! We are based in St. Louis, Missouri.
In 2001, the only medication we could use to treat opioids was naltrexone (methadone can only be given at a state licensed clinic) and again naltrexone and disulfiram to treat alcoholism. My expertise in using naltrexone came very handy. The success of my clinics was based on medical detox, and naltrexone administered under direct observation (2 tabs on Monday, 2 tabs on Wednesday and 3 tabs on Friday). I would go to great length training my physicians on naltrexone and even more time on educating my patients on the opioid ‘blocker’ that was going to turn them into a zombie and destroy their sex life! The analogy was used was the ;crutch’ or ‘cast’. You need a crutch or cast for the bone to heal. I like Marc analogy of the scaffolding. My bigger challenge was reassuring and retraining the therapists and counselors, most of them in recovery and vehemently opposed to any medications, I cannot tell you how times well-meaning but ill-informed therapists convinced the patients to stop naltrexone.
The ideal dose of naltrexone to treat alcoholism is 100 mg daily (study COMBINE). Our physicians would encourage patients to carry naltrexone with them and pop an extra pill if strong craving emerged in the evenings, while on a trip etc. Cravings is like allergies. Most of us learn to control allergies by taking an antihistamine pill appropriately.
The introduction of buprenorphine in 2002/03 gave us a new double-edged sword. It had to be used carefully and required spending a lot of time educating, yes physicians and patients on the pharmacology of buprenorphine and why naloxone was added to the formulation of Suboxone.
The other big issue is what is abstinence. I tell my patients that it can be a two-phase approach. The first phase is stop using the offending and illegal or illegally obtained substance. This usually applies to opioids. When patients start using opioids and do well on buprenorphine (methadone if they are getting it at a clinic) they are abstinent and can stay on buprenorphine indefinitely. Very few patients want to be on buprenorphine indefinitely. the vast majority (95%) of our patients on long-term buprenorphine are older and in chronic pain. If these patients want go the next phase of getting off buprenorphine, we offer them naltrexone and many do. We encourage patients to stay on naltrexone, including the monthly injection of naltrexone sold under the brand name Vivitrol for 2-3 years or longer. The key success step of long-term recovery is attending group and individual counseling. The advantage of attending groups is if a slip occurs we can help them pretty quickly.
Abstinence is patients with alcohol use disorder is a little tricky. The ideal situation is for the patient to quit alcohol completely and many do, but not all. The first step is getting patients to cut down. Naltrexone does it splendidly. Patients drinking 8-10 drink a day are down to 1-2 and then quit, Other’s quit and may have a slip and get back on the train. We have a small number of patients who take naltrexone and have 1-2 drinks a day. We don’t make a big deal about it. There are patients who want to be on naltrexone and disulfiram and others want to be on disulfiram and accommodate these goals.
The question I get asked often is the Sinclair Method. I knew David Sinclair and we had some very interesting exchange and live talks. His method encouraged patients to take naltrexone only the days you were going to drink. We found this not too practical. We encouraged patients to take naltrexone on a daily basis. We have several patient insisting on trying the Sinclair Method and we are fine with it. I cannot sufficiently emphasize the key component of treatment — counseling, both individual and group. Easier said than done.
I end by a quote from Bill Wilson the founder of AA in response to his followers shocked on him taking LSD to curb his craving: THE PATHS TO RECOVERY ARE MANY,
Hi Percy. I read this with interest. Of course I know your work, and you’ve described your approach on this blog in the past, in great detail, for example here: https://www.memoirsofanaddictedbrain.com/?s=menzies&Submit.x=0&Submit.y=0 . But new readers may appreciate this summary.
I think the highlights of your approach are (1) the choice you afford your patients (in terms of which meds they want to try and what sort of schedule they prefer) and (2) your insistence that medication-assisted control or abstinence has a far better chance of working when combined with counselling.
You also have a gentle way of understanding addiction and recognizing it as a condition that need not define a person and need not last indefinitely. You have written before about cutting off access as a silver bullet for opioid addiction. You obviously realize that this is a socioeconomic issue that simply can’t be resolved by good intentions…and is virtually impossible (and probably undesirable) for alcohol. So…what’s left? Naltrexone, a second-line silver bullet that pulls the rug out from under craving.
I applaud your approach (though it differs from my own) especially for those who can’t find another way. Your resolve and your energy are admirable!
Hi Colin,
Good to hear your thoughts, I and can offer this view from someone who’s feelings have changed and no longer feel addicted.
I would describe this in a different way:
“Some people who have learned to become indifferent to alcohol “,
This change is feeling-based, and it “occurs” rather than something that is done or learned. The struggle and recovery work is certainly headed toward this change,
but if it occurs or not, is not due to doing it or learning it.
For instance, most people have had a favorite writer, composer, sports team, etc,, that they had strong feelings for, but have found those strong feelings wain, or even disappear altogether.
The how and why can be reflected on, but the point is that the change, “occurred”.
The feelings may change back again, but it cannot be learned or decided.. it occurs.
Dear Marc,
You summarize my treatment philosophy very well. Easy access to the offending substance and low prices are the two dominant factors contributing the spread of addiction and making recovery so much more difficult. In today’s context, I describe addictive disorders as socially contagious epidemic. The ‘pathogen’ is the drug or alcohol and the vectors spreading the contagion are easy access and low price.
The present lockdown in the US is a good example on how the pathogen of addiction is spreading..Liquor stores are considered ‘essential’ services and allowed to remain open. Sales have increased over 50% and the calls for help have gone up.We fear alcohol sales will go up even more when the stimulus and unemployment checks start arriving.
The ‘silver bullets’ for helping people get off drugs or alcohol is humanizing the treatment and making it attractive. We have demonized, criminalized, medicalized, moralized treatment but the missing component is humanizing the treatment. The other missing component is making treatment attractive. I often remind my staff about our competitor – the drug dealer! What are we doing or not doing that makes the patient go to the drug dealer? If the medical detox is done right and the patient feels well; if the right dose of the maintenance medication is prescribed; help with jobs, job training is provided, the patient is likely to remain in treatment. This approach has worked very well for us and I am not surprised at ARCA being the biggest provider of medical treatment in Missouri.
Colin,
Your Habit-Language analogy is logical and makes sense, but would add an element.
From a former addicts point of view who experimented with drinking, including a blackout (in a safe place ),
I found that the ultimate feelings of relief, freedom and “bliss” did not occur as they used to every time I drank to blackout for decades.
I realized I was no longer, “in love” with the addictive substance.
This blackout experience was like trying to make an old relationship, “work”, but the feelings of the heart had changed.
Nor did drinking instantly spark, “the old habit and lifestyle” like it had in the past as the many “relapses” had in the past.
I feel fortunate that a “change of heart” occurred at some point, but do not feel it was “accomplished” or “done” by me…it “occurred”.
I think what you are saying about habits can help point people in the right direction, but
addiction, like love, seems to be ultimately a matter of the heart.
So if and when people fail in their habit/learning efforts, this notion that it is a “matter of the heart” may help them know its not from their lack of trying. ( I am sure a lager percentage of addicts would agree, but there has been no venue to express this.)
There have been MRI studies of the changes of feelings of love.
I think these could shed new light on the understanding of Addiction and what recovery is, if former addicts like myself were studied. (it is not simply “not engaging with an addiction”).
“like trying to make an old relationship, “work”, but the feelings of the heart had changed.
Nor did drinking instantly spark, “the old habit and lifestyle” like it had in the past as the many “relapses” had in the past.
I feel fortunate that a “change of heart” occurred at some point, but do not feel it was “accomplished” or “done” by me…it “occurred”.”
This is a very relatable experience to my own ♥️ it!
Great to hear.
Perhaps accounts from people that no longer feel triggered” could offer people something new to consider if the disease model and other models do not resonate with them.
The “change of heart“ seemed to happen after a series of “realizations” like what people have for other things.
It was strange when I realized that those instant feelings of freedom, relief, and bliss was no longer occurring when drinking.
It was somewhat like meeting a significant-other that you wanted to break away from.
If it occurs, profound feelings and perceptions have “changed”.
Although a great relief, there is also a strange feeling of wonder and reflection.
The point being is that these changes seem to ultimately be in the arena of the feelings of the heart.
But how is this scientifically and/or medically described, treated, or even tested for ?
Hi Carlton. The system – or my computer – seems to be delivering again. Thanks for your insights. I agree with you that change can happen in a number of ways and that sometimes, one way is much more important than the others but that’s often apparent only in hindsight. I also agree that change can just ‘happen’ for no obvious reason. As long as the change is in the right direction and sustained, then at one level the reason doesn’t matter much to the patient but it does matter to researchers, who want to know which approach to change is most likely to work for most people – or for particular sets of people.
Comparisons with ‘love’ are probably not much help to researchers because it means very different things to different people – and sometimes to the same person at different times. We can all agree that it’s a powerful emotion but unfortunately, its effects are not always beneficial. Ask any disappointed lover.
As I’ve mentioned in an earlier response, I feel strongly that patients should be involved in choosing from the range of evidence-based treatments and treatment goals, which includes both harm reduction and abstinence. Some patients need both those approaches at different times. For example, with opiates, where withdrawal can take much longer and be much more unpleasant than with alcohol, an abstinent patient who has a relapse after stopping naltrexone may not be able to take time off from a new and crucial job to detox again, much as he or she might like to. In that case, a few weeks or months back on methadone or buprenorphine can maintain the basic treatment goal (abstinence from heroin) until the job is secure enough for them to take a therapeutic ‘holiday’ and get back on naltrexone.
Similarly, some people need a lot of therapy while others manage lasting change without much more than occasional contacts where all I had to do was listen to their happy accounts of progress and make encouraging noises.
I have very little experience of non-chemical addictions, such as gambling, though I did one of the earliest studies of weight-loss surgery, which seemed – back in 1975 – to have surprisingly few psychiatric side effects and worked well even in people with a psychiatric history. In contrast, I think we are far from finding a universal anti-addiction drug. Naltrexone has been touted a bit in that respect but there are a lot of negative studies and as I used to point out to my students, the history of medicine is often the history of good ideas that turned out not to work, not to mention the bad ideas that had no chance of working, except at a placebo level.
Colin, Thank you for this detailed reply and will post a detailed follow-up soon, but in the mean time,
Two quick questions about Disulfiram, which (fascinatingly) eases “the endless internal arguments”, rather than just causing an unpleasant reaction to alcohol, like Antebuse.
1) Do you know if disulfiram has been used or tested for no-chemical-based addictions? (It seems it would be ideal for them).
2) Have there been reports of side effects with Disulfiram? I am curious of other types of “the endless internal arguments” that people experience, are also effected.
Thanks,
Carlton
There is a single case report of an alcoholic with a gambling problem whose gambling stopped when disulfiram was added to his treatment. (Mutschler J, Bühler M, Grosshans M, Diehl A, Mann K, Kiefer F.
Disulfiram, an option for the treatment of pathological gambling?
Alcohol Alcohol. 2010 Mar-Apr;45(2):214-6. – discussed in my book.) However, it could have been due – and in my view, probably was due – to non-specific factors. Since gambling is quite a common co-addiction in alcoholism, I think it would have been noticed in the 70+ years that disulfiram has been used if an effect on gambling – or other behavioural addictions -was real rather than coincidental. When alcoholics stop or moderate drinking – however they do it – there are usually large improvements in other areas of their lives.
As to side effects, as drugs go, Antabuse is not notably toxic. It only has one potentially lethal one (acute liver failure) but it is very rare and always survivable if the drug is stopped as soon as signs – particularly, dark urine – appear. I never saw even a single case in 40 years of prescribing. Other side effects are equally reversible. Compared with the organ damage caused by continued heavy drinking, the toxicity of Antabuse is negligible. As one researcher noted, it is safer than aspirin. That also applies to the very small risk of death from the reaction with alcohol. I always mentioned that risk to my patients but always added that it would be a very unpleasant way to attempt suicide and very likely to fail.
Hi Marc, is it time for us to have a conversation about tobacco and nicotine, and novel approaches to cessation? I know how you like and appreciate innovation, being a trailblazer yourself.
Let me know if so.
I’m (at long last;) ready!
Joanna
Joanna, I’d welcome it if you’d discuss this in the context of the present post. Are you suggesting there are substances that help people abstain? Last time I checked, the nicotine patch had a success rate below 20%. Can you bring us up to date?
I’m not much for the substances, in and of themselves.
Goodness, how many times have I heard someone say, “I’m using the gum/patch/lozenge, or such and such medication, but I’m still struggling a lot…”
I think, Of course you are! That’s not even close to enough support for something you’ve been dosing 200 times a day.
it’s more about having a multi-faceted response to the challenge, and recognizing that we need that, so that we seek out, invite and welcome that support, in ALL its forms: medicinal, human, habitual, nutritional… on and on.
One of the most abused and readily available drugs is actually alcohol. Most people don’t know what professionals in the rehab industry know: alcohol is the dirtiest drug.How Long Does Alcohol Stay in Your System?
Colin,
In a way, your approach is like Detox, but without the Brick and Mortar.
I am curious if you tried this method with other addictions, such as Gambling, video internet games, shopping, etc, etc.
Best,
Carlton
Hi Carlton. I wrote a long reply to several of the posts (including yours) but it got lost in cyberspace. I will reconstruct it and try again – and this time, I’ll save a copy.
Hi Colin,
It sounds like you inform your patients of what is available, and can choose and try procedures.
I would like to offer this sentence that may resonate with a percentage of your patients.
(please re-word if it could be clearer ):
Sustained attention is a trait of addiction, and also occurs when love arises.
As a former addict, they were one and the same.
For people that innately feel addiction is neither a disease or a disorder, this may help them comprehend their situation, and help in their recovery efforts.
Hi Colin,
I re-read your post and would like to offer one more thing since the blog has moved on.
Your logic , common sence and habit/language analogy can give patients hope and something to look forward to.
But another part of addiction are certain types of irrational thoughts and beliefs that occur.
These “matters of the Heart”-type things but can change, and even suddenly, but it is an internal thing.
Colin, you are also right that this type of description is not helpful for researchers, but perhaps just by mentioning this to patients, it may help relieve feelings of destitution and failure when relapses occur.
I find this so true, my father was a chronic alcoholic for 30 years and after 5 years of sobriety started drinking again after a cancer diagnosis. I know that it had nothing to do with cancer it was his choice, the cancer was an excuse, but his drinking never became daily like before, because after the cancer treatment his body could not take the abuse of alcohol. Once again he chose to drink when he felt like it , it was hard core drinking but only for 2-3 days then he would stop, the cancer treatment was his Antabuse, this always confused me until I came across this website and came to the conclusion that my father could of stopped drinking a long time ago and used the addiction model of alcohol abuse to further his drinking because he thought he was diseased and therefore not at fault.