…by Nick Jaworski…
After nearly 80 years, addiction treatment in America is slowly warming to the idea of multiple pathways to recovery, after viewing the 12 steps as the only “real” way to recover. MAT (medication-assisted treatment) is among the most promising.
This is a guest-post by Nick Jaworski, owner of Circle Social Inc., a marketing and consulting firm specializing in addiction treatment. (See bio information at bottom)
……………………
Quite recently, MAT has gained recognition as the gold standard for care in treating opioid use disorder (OUD) among researchers, legislators, and even the general populace. But the acceptance of MAT by the professional treatment community has not been nearly as fast.
Many providers I speak with are still very reluctant to accept MAT in their centers or as a viable component of treatment within the field in general. Even if facility leadership is on board, there’s a good chance staff or referral partners won’t be.
Other providers, such as Hazelden, were also reluctant at first but looked at the research and made their own determination that they had to change their approach (other providers, even today, still look down upon them for it).
Congress and many States have also recognized the efficacy of MAT and so have begun to pump serious money into programs that offer it (like this large grant from SAMHSA). Insurance providers often prefer MAT as well.
Cost is a very significant factor for legislators and insurance providers. MAT protocols can be provided to those struggling with opioid addictions at a fraction of the cost of a residential program ($4,000 or less a year versus $28,000 a month for your average residential program).
Since the majority of those struggling with addiction lack resources or are on Medicaid, MAT also opens the doors for the demographic with the greatest need to access care.
There are two additional drivers of the increase in the use of MAT in the US — Wall Street and parents.
Wall Street has seen great opportunities because the opioid crisis is constantly in the news and the addiction treatment industry has an estimated market cap of at least $35 billion per year. These investors come from outside the field and do not have the same biases. They look at the data and see what’s effective and where trends are going.
And then there are the parents referring their adult children into treatment. Many parents, especially mothers, have become completely disenchanted with the addiction treatment industry as it has existed since the late 1990’s.
Their Children Are Dying from Overdoses, and Parents Aren’t Taking It Lying Down
 The bottom-line is that length of care is one of the highest predictors of success for treatment, so any 28- to 90-day program has very slim chances of success for the first round or two of treatment, regardless of what model they are using. To move away from abusive substance use requires extensive development of new neural pathways that drive new habits and patterns of thought.
The bottom-line is that length of care is one of the highest predictors of success for treatment, so any 28- to 90-day program has very slim chances of success for the first round or two of treatment, regardless of what model they are using. To move away from abusive substance use requires extensive development of new neural pathways that drive new habits and patterns of thought.
As outlined in my article on a Brief History of Addiction Treatment Marketing, it was not uncommon for these young adults to go through 10-plus rounds of treatment. My team and I actually just interviewed a client who was currently on his 27th round of treatment!
As you can imagine some parents have become extremely skeptical after 10-plus rounds of failed treatment (not to mention that they’re paying as much as $30,000 a pop). But, more importantly, many parents have lost children to  opioid overdose. The 18-26-year-old age demographic has always had the highest prevalence of drug and alcohol abuse. Most of the time, this is alcohol or marijuana, with smaller percentages using meth, cocaine, and other substances.
opioid overdose. The 18-26-year-old age demographic has always had the highest prevalence of drug and alcohol abuse. Most of the time, this is alcohol or marijuana, with smaller percentages using meth, cocaine, and other substances.
 However, with the rise in availability of opioid-derived prescription pills, more young adults were switching to these painkillers, which have a high potential for overdose when mixed with other drugs. A subset of these users would go on to heroin, especially when prescription regulations reduced the availability of legal drugs. As most readers know, the extremely high overdose rates of the last few years have been driven primarily by fentanyl-laced (or -replaced) heroin. Unlike
However, with the rise in availability of opioid-derived prescription pills, more young adults were switching to these painkillers, which have a high potential for overdose when mixed with other drugs. A subset of these users would go on to heroin, especially when prescription regulations reduced the availability of legal drugs. As most readers know, the extremely high overdose rates of the last few years have been driven primarily by fentanyl-laced (or -replaced) heroin. Unlike  in the past, when young adults using drugs or alcohol mostly survived to go on and live normal lives (probably like most of those reading this blog), these kids were dying instead.
in the past, when young adults using drugs or alcohol mostly survived to go on and live normal lives (probably like most of those reading this blog), these kids were dying instead.
So parents were sending their children to multiple rounds of rehab, paying tens of thousands of dollars, and then losing their children to overdose anyway. As you can imagine, this created a lot of anger and resentment.
But that was nothing compared to the anger many parents felt when they learned there was this option called MAT that decreased overdose deaths by roughly 40-60% and they had never heard about it! It’s not uncommon for parents who have lost a child to overdose to tell me that the first time they’d heard about MAT was after their child’s death.
Imagine how you would feel if you sent your child to the hospital and you weren’t even told of a readily available and cost-effective method of preventing your child’s death because the doctor personally didn’t care for the treatment.
This is the kind of anger we see from parents such as Gary Mendell, who created Shatterproof, or Justin Phillips, who created Overdose Lifeline. Parents are simply giving up on the traditional rehab industry as a whole because they feel lied to.
American Addiction Treatment Perspectives Are Shifting, But in What Direction?
All of this has started to open the window to different conversations surrounding effective addiction treatment. Programs relying solely on 12-step and abstinence-based models are regularly being called into question.
However, I am not yet seeing an attendant shift in the disease model of addiction. Conferences premised on non-disease models are still small, and advocates of this approach are still few and far between.
 I am on the board of Above and Beyond Family Recovery Center in Chicago, one of the most innovative treatment programs in the country. We focus on providing free, high-level outpatient treatment to Chicago’s homeless and disadvantaged, but we have had a hard time gaining the support of other treatment programs in the city because we do not focus solely on 12-step programming or disease models of treatment (although these are offered alongside our other programs).
I am on the board of Above and Beyond Family Recovery Center in Chicago, one of the most innovative treatment programs in the country. We focus on providing free, high-level outpatient treatment to Chicago’s homeless and disadvantaged, but we have had a hard time gaining the support of other treatment programs in the city because we do not focus solely on 12-step programming or disease models of treatment (although these are offered alongside our other programs).
 Americans have a long history of deterministic thinking when it comes to human behavior. Starting with Calvinistic predeterminism in colonial America and then evolving into Eugenics, the American view of genetic influences rarely goes beyond a limited and simplistic notion of Mendel’s pea experiments (perhaps a topic for a future blog post).
Americans have a long history of deterministic thinking when it comes to human behavior. Starting with Calvinistic predeterminism in colonial America and then evolving into Eugenics, the American view of genetic influences rarely goes beyond a limited and simplistic notion of Mendel’s pea experiments (perhaps a topic for a future blog post).
With this misconception, most Americans still view addiction as some kind of genetically predetermined disease, one that is chronic, progressive and incurable.
In the context of our conversation here, MAT is seen as some kind of fix for an ingrained defect, one that perhaps rebalances out-of-whack or deficient  neurochemicals in the brain. What most Americans have not yet grasped is that MAT, or any other substance that alters the brain’s neurochemicals, simply combats symptoms, which is not so different from how cold medicines alleviate symptoms rather than cure the actual cold. The key difference here is that OUD symptoms induce so much suffering that users are often driven to continue using. Opioids are of course the best (if not only) way to control opioid withdrawal symptoms. In this respect, relieving symptoms, though not a cure, can change behavior patterns that exacerbate the underlying problem.
neurochemicals in the brain. What most Americans have not yet grasped is that MAT, or any other substance that alters the brain’s neurochemicals, simply combats symptoms, which is not so different from how cold medicines alleviate symptoms rather than cure the actual cold. The key difference here is that OUD symptoms induce so much suffering that users are often driven to continue using. Opioids are of course the best (if not only) way to control opioid withdrawal symptoms. In this respect, relieving symptoms, though not a cure, can change behavior patterns that exacerbate the underlying problem.
In order to truly find recovery, you must rewire the neurological pathways in the brain, which will, in turn, drive changes in neurochemical balances. Just as one cannot lose weight or get fit by taking a diet pill, individuals cannot overcome addiction by taking a prescription. The pill can help, but lasting behavioral change requires focused effort over extended periods of time, as Dr. Lewis has often pointed out.
It is only through an accurate understanding of the interplay between genes, environment, and human experience that we can create effective solutions which help individuals and communities. It’s a goal I strive towards every day and I hope others reading this will do the same. For a much more in-depth discussion on how unconscious processes involved in learning and development (rather than genes or choice) drive addictive behaviors, see my article You’re Thinking about Addiction and Choice All Wrong.
………………………………
Nick Jaworski is an internationally recognized executive in the field of behavioral health marketing and operational consulting, with experience building organizations world-wide. As the owner of Circle Social Inc., he has helped healthcare organizations perform turnarounds and accelerate growth. He and his team spend most of their days in and out of treatment programs across the country. They do extensive analysis of trends, observe programs, interview patients and families, and analyze data from marketing campaigns. Nick is an advisor to the board for The Behavioral Health Association of Providers, and is also on the board for one of the most innovative treatment programs in the country – Above and Beyond Recovery.
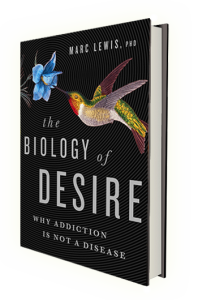 Informed by unparalleled neuroscientific insight and written with his usual flare, Marc Lewis’s The Biology of Desire effectively refutes the medical view of addiction as a brain disease. A bracing and informative corrective to the muddle that now characterizes public and professional discourse on this topic.” —Gabor Maté, M.D., author of In The Realm of Hungry Ghosts: Close Encounters With Addiction
Informed by unparalleled neuroscientific insight and written with his usual flare, Marc Lewis’s The Biology of Desire effectively refutes the medical view of addiction as a brain disease. A bracing and informative corrective to the muddle that now characterizes public and professional discourse on this topic.” —Gabor Maté, M.D., author of In The Realm of Hungry Ghosts: Close Encounters With Addiction
Makes sense working with the whole issue along the whole continuum. It takes as long as it takes and whatever it takes. It’s realistic and pragmatic and should be the mainstay of any integrated approach! Thanks
I really appreciate and embrace “recovery” as a “process” and not an event for sure. It is so very important to influence the neuropath ways in order to adopt a whole new way of being, thinking and/or behaving which sustains change/becomes the new norm. Long before I developed a “drinking problem” I had developed a “Thinking Problem” about drinking. Once the alcohol was introduced “like magic” I was hooked-in. Removing the alcohol, in my opinion, was only dealing with the symptom of my Thinking Problem. However, over time, and actively involved in the A.A. Program my Neuropath-Ways were influenced. It was the modeling that took place and folks sharing similar struggles together like a “family-of-affiliation” that really impressed me. So! in many respects, this was more of a “discovery process” versus a “recovery process”.
I also believe Medicated assisted treatment is essential in terms of savings lives especially with the risk of overdose from using Fentanyl or Fentanyl-laced drugs etc. Hope and recovery, or perhaps “discovery”, is open to the many possibilities of healing and health not stuck in the past. Changing neuropath-ways isn’t just for patients or “clients” but is also extremely important for treatment facilities and/or systems.
Thanks!~
I really like that comment on AA Gary. It’s a good connection I think a lot of people miss. When AA works, it’s because of that rewiring. “First thought wrong” is a great example. People have built up pathways connected to their experience surrounding abusive use and that’s what they’ll default to until a new pathway is built. So “first thought wrong” is actually a great CBT technique to stop, think about your thought process more consciously, and then decide if you need to change it. Do that long enough and you’ve built a new default pathway!
Another aspect of AA that works incredibly well is the community aspect and, as you mentioned, the modeling. Much of our neural wiring is influenced by those around us.
Thanks for presenting this – I too wish there were more providers who would buy in. I have a cousin who works for a company that manufactures cutting edge technologies in the medical equipment field and he told me several years ago that studies had proven MAT is incredibly more successful. My own son has been in treatment for over 4 years and is working towards discontinuing the medication within the next year or two. He is on a very low dose now and has found it extremely helpful.(In his particular case though he also found he had to move geographically to escape the “people, places, things” aspect of addiction). I feel badly though for many people who cannot afford the treatment. There are many addicts who are, simply by virtue of their addictions, unable to work and therefore uninsured. I suppose that’s the next threshold needed to cross. Meanwhile, where is the pain medication that supposedly was being researched that would NOT have addictive properties? I suppose big pharma is not as anxious to bring that to market……
Please, can we stop calling it medication *assisted* treatment, when it is very clear that the medication is the component that reduces the death rate by 50% or more? We don’t have “medication assisted treatment” for depression—we have medication and talk therapies and some people are fine with just meds, some are fine with just talk and some need both or vary over time. Same is true here and this is just silly.
The National Academy of Medicine recently urged this change as well:
http://www.nationalacademies.org/hmd/Reports/2019/medications-for-opioid-use-disorder-save-lives.aspx
Also, Big Pharma has been looking for a non-addictive opioid ever since it thought heroin was a non-addictive replacement for morphine, it’s a genuinely hard problem!
While I do agree with you that the medication is an important component in terms of preventing overdose and saving lives, I disagree that we should remove “assisted.”
I’m actually speaking on this topic at the National American Mental Wellness Conference coming up in PA in November. There is a false assumption in the US, which you’re echoing here, that the pills are the fix, because the entire emotional or regulatory problem is stemming from some kind of balance issue or chemical deficiency. This is incorrect.
There are feedback loops between the neurochemicals and the neuropathways, so there is an interaction process here, but prescriptions can only modify symptoms, not change the underlying neural pathways causing the issues. What a pill can do, just like methadone and bup do, is provide an opportunity for clarity, to re-engage the PFC, and build out new pathways.
To use depression as an example, if you’re so depressed you can’t get out of bed or are constantly engaging in suicidal thoughts, an SSRI can push you into a state where you have a positive enough mental state to now engage in the hard work of changing pathways so that, eventually, you could stop the SSRI if you wished.
Related to your comment, the major misconception is that we do not describe depression treatment using SSRIs as MAT. We absolutely should as that would be a more effective conceptualization. Your brain isn’t broken. It’s operating completely normally according to everything we know about neuroscience. The problem is that the current configuration is not optimal for living a successful life as the broader culture would define it.
So building out new modes of thinking and behavior through therapy, springboarded by prescriptions as needed, is engaging in that same standard process in the brain. The same processes that created the downward spiral can lift you right back out.
Well put, thank you. I’m a senior who is stuck in overeating and it’s very very hard not only to lose weight but to change my habits.
This theory of changing pathways makes a lot of sense and may even help me in getting off zoloft. When I tried tapering off with my family doctor’s help some years ago, I came to a dark place emotionally and physically. I could barely move, plus dark thoughts inhabited my mind all day – suicide, meaninglessness and such – my doctor told me that most probably the circular reuptake thingies in my brain were not usuing the existing serotonin efficiently. Does this make a difference for some people? But in any case you make a persuasive argument and there is hope.
Hi Larissa. There is certainly hope. The best way to change pathways (of thinking, of synaptic connection, etc) is to direct your energy and motivation to something else, something different. It is indeed hugely difficult to try not to do something…much easier to try to DO something, and let the “undoing” be a side effect.
It’s not like I just read this now (lol), but I’m replying now.
Good point – I HAVE been trying to not do something.
thanks again for running this forum, it’s so helpful
I still disagree. There is no evidence that *forced* counseling adds anything other than costs. Obviously, most people with addiction will benefit from all types of support from housing to job training to psychiatric care— but those “assist” the medication, which is the thing that reduces mortality. And not everyone wants or needs those things— they should be triaged to the people who *do* want and need them. Medication can be harm reduction or stabilization— we need to meet people where they are and provide what they are ready for, not what we think they should do.
We have a deadly overdose crisis and these theoretical wonderful supportive counseling groups that people are being forced to participate in are a barrier to saving lives. And, they are much better in theory than in practice, as anyone who has ever been on methadone can tell you.
Addiction is the only condition for which we *require* people to participate in other treatment in order to get lifesaving medication. Do you want to be forced to show up for mental health care that you don’t find beneficial in order to get your Prozac? I sure don’t.
Doing anything different for people with addiction is infantilizing and dehumanizing. Oh, and also ineffective— do you really want to sit in a group and talk about being abused as a child when everyone else there is watching the clock?
I think we’re referring to two different points.
– Must behavioral therapy be a requirement to receive medication? No, the research is clear that the prevention of OD is the same with or without therapy in the short-term.
– My point is that medication should not be considered a fix or sole solution as it’s unlikely to be effective long-term (though short-term studies are positive).
In terms of coercing in to treatment, I agree that it’s not beneficial, though there is some data suggesting that recovery rates for those forced into treatment vs. not are the same. I’ve seen studies stating the opposite was well, so jury is out there from a research standpoint. However, my gut sense is that coercion is not as effective.
Maia, who said anything about “forced”? The most effective treatment programs, I think Nick and I would agree, offer decision trees at every step of the treatment process. The trajectory of treatment should always be negotiated between client and treatment provider. And of course counselling-free methadone should always be an option for opioid addicts.
The newer models are founded on harm reduction principles, not a misguided insistence on abstinence. I think you’re arguing with a favorite phantom here.
Also, since you brought up depression meds, let’s recall that the effectiveness of SSRIs is minimal if not nil for many people. I agree with Nick that depression meds are most often useful as a bridge. Since both opioid addiction and depression are consolidated through emotional, physiological and behavioural elements, and both can lead to premature death, combining pharmaceutical and psychological approaches to intervention may be a useful general model.
Sitting around looking at the clock, or looking at people looking at the clock, is obviously useless. Nick and I met at Andrew Tatarsky’s centre, where psychological treatment is far more sophisticated than your state-run rehab is likely to provide (though that raises other difficulties, e.g., when it comes to who’s paying).
P.S. It’s very nice to talk about theoretically rebuilding thinking patterns and self regulation, but that’s very hard to do when someone is dead.
Everyone pretends that this stuff is just about getting decent care to people— but in the real world, the idea of “medication assisted treatment” is used to support the current system of requiring people to get counseling, etc. in order to get meds. Try visiting a typical methadone clinic or look at what happens to buprenorphine patients who don’t want counseling.
I’m not talking about old phantoms, you guys are ignoring the real hassles that are imposed on patients in the name of treatment having to be “assisted” if you are going to get medication.
That is the reality: the reality of emphasizing that people need more than just meds is supporting a coercive, harmful system that is far from optimal.
Okay, point taken. But you are talking about the public health system in one very particular country whose public health system is famous for its deficiencies. You’re talking about life on the ground in American inner cities. Sure, it’s important to report on how certain practices are used and abused by specific social/economic interests. But it’s far from the big picture.
Also, I really wish that you’d occasionally remind people that you’re talking about opioid dependency — a physiological dependency with nasty withdrawal symptoms. You don’t address “addiction” per se. I’m not mincing words. There are vast numbers of meth, coke, and alcohol addicts (not to mention porn addicts, food addicts, and compulsive gamblers) for whom these sweeping admonitions have no meaning.
PS. You know I’m a fan of yours.
I can see your point about requiring counseling to get meds in the sense that it’s not required for other treatments and the meds, in this case, are often life saving. So I’ll agree with you there.
But that topic isn’t the focus of the article. One of the main points here, especially in our discussion in these comments, is that behavioral change is absolutely needed for successful recovery long-term, whether that’s done on one’s own or with professional help. The drugs alone simply can’t provide that.
Helping individuals and the broader culture understand that behavioral change is a long and difficult process that cannot be realized through meds alone is extremely important in order to institute more evidence-based practice. Also, there is a very large value in helping people understand everyone has the capability to change. They are not locked into some horrible destiny due to genes or current chemical balances in the brain.
So you’re right that current policies in the US are doing harm by not allowing people access to medication without other hoops to jump through, but we cannot simply throw out behavioral change techniques and supports because that’s currently the case as that would also be detrimental.
Death is not the end… we can change OUR thinking patterns, improve our lives, model for others, and give each other hope. Death is terribly final… but not the end. We must continue.
I will defer on the discussion about using the term “assisted” treatment. The controversy about concepts and advocacy that recognize the very important but limited role of psychoactive substances as an integral part of recovery is not new. I became involved in addressing the stigma around mental health and the recovery process 20 years ago. I think that an important element that needs to be emphasized is the understanding of the person in recovery about the role and function of medication in his/her recovery process. If the individual doesn’t have a real understanding of how medication assists in his/her recovery, then the use of medication is a passive process, with the provider being the one receiving the “assistance”. How about using “medication-empowered recovery”?
Ooo, I like that.
I like that as well. Thanks everyone for this rational, caring, thoughtful conversation. Empowering.
I hope I’m not naïve in thinking that every participant, of this particular discussion, holds in their best interest the health and welfare of those impacted by SUD and/or MHD’s. Getting “caught-up” in terms of semantics and/or terminology isn’t helpful or even hopeful. As I had mentioned in my previous post, perhaps real-change starts with our own neuropathways not being bogged down or narrow minded in thinking.
Regardless of ones’ perspective, the bottom-line is, we all want what is best for those impacted by addiction and/or mental health disorders.
In reflecting upon AA one of their great “proverbs” and/or sayings was; “first you come”, then “you come to” and then you come to believe.
I agree that perhaps a person suffering from an addiction or in severe withdrawal cannot grasp concepts such as CBT, at least in the beginning. Once stabilized though, with permission and as a joint partnership you may start to introduce the idea of better decision making, better coping skills, ways of thinking and behaving that enhance the quality of their lives.
Medication most certainly can and hopefully reduces the symptoms, however, as part of a continuum is a way of living with little or no dependence on meds ideally.
However, if ones’ culture of care is reflective of emergence due to a crisis or epidemic then it is reasonable to believe that getting medication is critical, this also makes perfect sense. Again, regardless of your lens, we all want what would be best, effective and long lasting.
Sure we do, Gary. But I don’t see this argument as getting stuck in semantics. What Nick, Maia and I are discussing are fundamental principles for helping people at perhaps different stages of opiate addiction. You seem to agree that readiness for psychotherapy and behavioural change may not appear until people achieve physiological stabilization. These are important distinctions, but I think semantics helps rather than hinders, as long as we are conscientious in how we use words.
why do we talk about “treatment’ at all – we’ve been sucked into the medicalisation of a behavior for years – what other behavior do we treat like addiction (or actually just plain drug use) – do we treat elite sportsmen who are addicted to their sport, or workaholics, or successful businessmen addicted to money – there’s big questions for mine over this whole idea
There is a certain value in moderation, particularly when a behavior becomes problematic for the individual or those around them. So while much of how we look at those who use is more judgment than objective observation, I wouldn’t do away with the word treatment. There are definitely times where people need professional help to get on the right track, no different than a math tutor or sports coach.
your are right too of course – at what point does a behavior go from an effective stress reliever to a potentially fatal addiction that needs treatment to in effect save a life. This too is where there is an element of disease in addiction even though i and others do not believe the overall behavior is a disease – at some point it becomes life threatening for some, not all – but too is the ‘treatment’ psychological support or indoctrination – are we seeking to alleviate distress or change a behavior to suit the moral police and the hypocrites in society who look down upon the less fortunate
Interesting topic, but I am a bit unclear.
People are “seeking help” on their own at AA, SMART, etc.
They initiate it, It is not assigned “treatment” per se.
Or are you taking about something different.
What on earth do you mean, Carlton? People seek — and find — treatment for everything from warts to crabgrass to bed-wetting. Treatment just means help by an informed or knowledgeable source.
Hi Marc,
For me,If you are getting “treatment”, the ball in the professionals hands…they are “treating’ you.
You are cooperating, not necessarily “doing”.
The term; “Treatment ” means a specific professional procedure and perhaps doses of pharmaceuticals designed to produce results.
Personally, I see my years in AA and SMART as self-seeking help or consultation, not “Treatments” for my addiction.
Are couples “Treated” for Marriage problems?..I just googled the term: “Marriage treatment” and the results switched to “Marriage Therapy and Counseling.”
I see your point, Carlton, and perhaps it’s a useful distinction. But have you ever had your lawn treated…for weeds…or you trees treated for bugs or fungus? You’re still the boss in these (and other) contexts.
Anyway, words often pack punches, so it’s helpful to know what associations come up for given words for different people.
For Maia S, the main offender was the word “assisted”.
drug and alcohol is one of the few areas where people are in many circumstances made to undergo ‘treatment;’ whatever that may mean – this is particularly true here in Australia where mandated treatment via the justice system is common – would we in another world force obese people to have treatment, those addicted to sugar, or even send them to jail because they eat too much to cover their trauma, at least some of them anyway – there’s a difference between someone seeking self change and someone being made to change because the society doesn’t agree with what they are doing on moral grounds essentially. we argue over terms a bit in drug and alcohol and rightly so, often because the terms become general rather than specific; like addiction and the assumption everyone who uses drugs is an addict
Great comment Terry. I agree. We mandate treatment because we believe the behavior itself is criminal, which is why we mandate jail for offenders of other crimes.
Addiction is often a value judgment against someone else’s lifestyle. At the same time, I’ve seen many people very grateful for being encouraged into treatment, however strongly. Treatment for addiction can save lives.
So while I side with my view in the first paragraph, I can see why people might side with the second.
I work with “disadvantaged poor” people for 25 years and my anger grows because here in New York they HAVE to go to groups to get suboxone and EVEN vivatrol injections!!!!!! There is no option for these people.
These people have no say over their “treatments”. They are told how many groups to
attend… based on an intake??? more groups is better ? Perhaps more groups is more money for these clinics?
It’s bizarre to get suboxone you must be “prescribed” groups. It’s an injustice.
I work with parolees and probation and courtMandated people… the courts and parole officers aren’t suppose to dictate treatment but they do. I have people being mandated and sent away from families and young children for 3-9 months to residential programs because but they had a few “slips” people or even sent back to prison for weed??? …, don’t we see we are destroying the new generations?
And I think TErry said… do we send someone for sugar addiction to jail…?
And mandated treatment doesn’t get people better not from what I watch… if anything I see more rebellion and more destructive… I don’t blame them.
Try comforting a person being ripped from their families ….
The more I do this as a “counselor” the more the word “treatment” makes me want to vomit. Sorry I know that’s strong but inside that’s how I feel. As well as “diagnosis” of symptoms that just label people. People don’t even know what the dx means except “there’s something wrong with you” …
The only thing that works for people is teaching self empowerment.
I do nothing except listen (which many providers these days fail to do) , ask what do you want to try….and provide unconditional acceptance, which is another word for a very old concept …aka be like a friend. don’t judge.
People get themselves better if encouraged that they have the answers.
Lastly, I don’t have a problem with the word “medicated assisted” but unfortunately I feel segregating it that way leads to underlying stigma and over regulation.
See some of my comments above, but I agree with you for the most part Alison. It’s not OK to deny people prescriptions without attending group. We don’t do that in any other situation.
We’ve also seen empowerment as a primary method of healing for people. We actually incorporate quite a bit of Logotherapy into our work at Above and Beyond.
If you’re ever in Chicago, would love to show you the program.
Alison-Wow! That was a piece of work right there. It is music to my ears and I sincerely appreciate your posting it! I find myself going back to read it over and over as I do with many of the writings on this blog. The more posts I read like yours-the more it gets me to believe that the field really is changing for the better.
Nice to hear that, Carl. Thanks for sharing the good vibes!
PS Nick what your doing is wonderful… by the way!
Sorry my anger swept me up!
If I lived in Chicago I would want to work there!
It’s nice to know you are out there and trying to empower people!
Onya Alison – if we had guards at chemist shops making people attend a group before they got their blood pressure tablets what sort of furor would that cause – some would call mandated treatment false imprisonment – but your right too Nick – in some severe cases mandated treatment should occur – how do we work out which is right – certainly it shouldn’t be decided by parole officers and other associated poeple who are on an agenda to rid the word of drugs – a hypocritical agenda when we consider very busy chemist shops ….
I’m just going to say AA sucks. I became addicted to meetings. Harmless? No because the meetings consumed my life. Then, when one day I missed one, they all figured I was out using. I probably was. Then the longer I went I realized there were some real “holier than thou” acting people.i don’t know the answer. Thank God opiates are NOT my problem.
Russell Brand interviews Gabor Mate. Definitely worth a watch …
https://www.youtube.com/watch?v=C-mJnYmdVmQ
Here is an interesting article in the NY Times today:
Seattle Has Figured Out How to End the War on Drugs
https://www.nytimes.com/2019/08/23/opinion/sunday/opioid-crisis-drug-seattle.html?action=click&module=Opinion&pgtype=Homepage
Working up a reliance on medications isn’t a character flaw or a sign of inadequacy, and it takes more than self-restraint to beat the issue. Mauling unlawful or certain expertly endorsed medications can make changes in the brain, causing astonishing longings and a drive to use that makes the equalization seem, by all accounts, to be an amazing goal. However, recovery is rarely inaccessible, paying little respect to how hopeless your condition shows up or how much of the time you’ve endeavored and bombarded beforehand. With the right illicit drug use treatment and support, change is possible.
Thanks for your input to this blog, I think it is right on target. For a long time I have felt that my drug use (meth) was in no way a disease. I have always felt that it was as a result of living in a very chaotic and unsafe environment and by God you better be on your toes at all times.The consequences of not being in a perpetual level of readiness/hyper vigilant at some point becomes constant terror. In my experience probably the highest form of anxiety one can submit or unwillingly expose themselves to. That description above is no disease it is a learned tool and behavior for survival that gives the facade of safety for a young person or even a child. And leaves you in many ways as a child stuck in a survival mode in an adult world and this mode works less and less and is exhausting to the now-addict. And that spiderwebs out to all around them especially to those closest to them. Kind of an odd man/woman out. I hope that this makes sense and adds to the relevance of this blog. I’ve never have written in a blog and hope I don’t come off as a fool.
Your perspective is appreciated, John. Feel free to comment whenever you like. Note that comments on more recent posts are more likely to get replies, but lots of people read these things, so don’t worry about sounding like you’re off base.
I feel like we have people who think that smallpox was no big deal screaming back and forth at those who think we all need to be vaccinated against head colds – while those of us in the middle are just screaming into the wind.
Thanks for letting me vent. I agree with everything you said…and I am firmly in the middle ground on vaccines.
Help other people stay healthy through example, and slowly help increase the community’s health, nutrition, knowledge, and consumption of sustainably produced foods. Mark’s blog (not to mention other good food/health blogs) is a great example of this; his information and personal lifestyle add credence and interest to the posts.
I agree that perhaps a person suffering from an addiction or in severe withdrawal cannot grasp concepts such as CBT, at least in the beginning. Once stabilized though, with permission and as a joint partnership you may start to introduce the idea of better decision making, better coping skills, ways of thinking and behaving that enhance the quality of their lives.